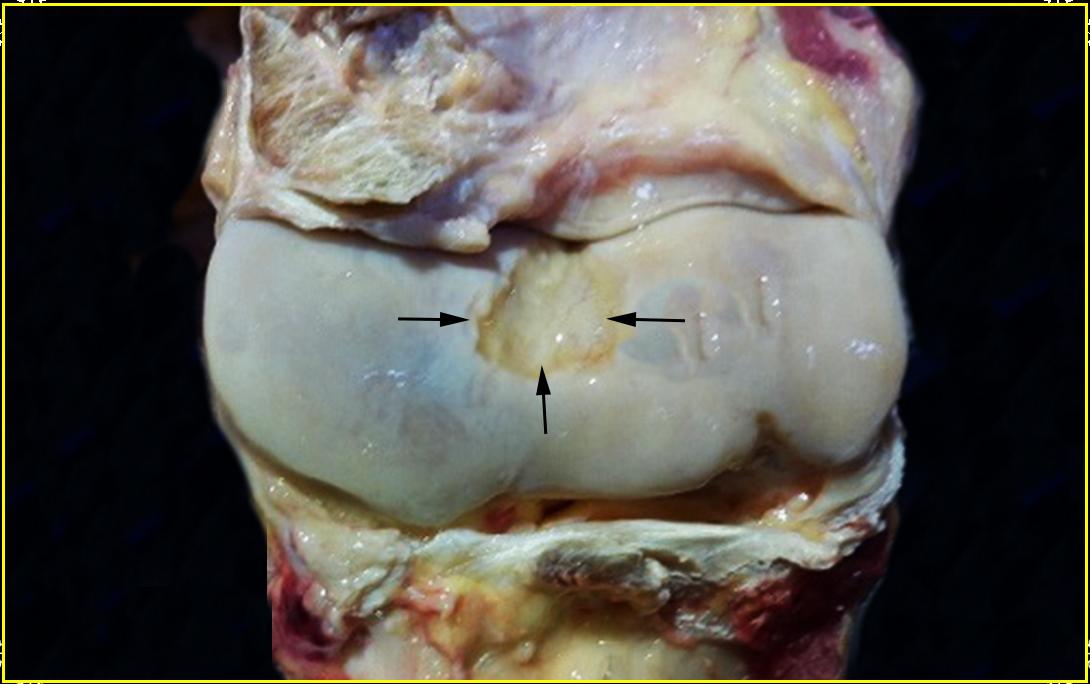































The above is a photo of an equine humerus (elbow) that has arthritis. I have seldom found shoulder or elbow damage in my racehorses and view such lameness as rare, but certainly this autopsy specimen tells me it may be more prevalent than I suspect. The joints of the racehorse are probably the most violated structures in veterinary medicine on a consistent basis. Even in my personal experience and I tended to avoid using vets any more than absolutely necessary, I have had more joints routinely injected than any other procedure performed on the backside. Accordingly, I have developed some controversial ideas on this subject which you might find food for thought, if not actually useful in your barn. The term, arthritis, means simply inflammation of the joint. To my way of thinking, joint inflammation is basically only caused by two things, trauma from athletic performance and infections or, perhaps more predominately, a combination of the two.
As with all things in life, one really needs to examine the complete structure for a full understanding without becoming to myopic from the details and in this case, that includes the:
1) hyaline cartilage,
2) bone,
3) near-by ligaments / tendons
It is the prevalent wisdom of the veterinary establishment that only bone can repair itself through remodeling . It is likewise taught in medical and vet school that cartilage is virtually irreparable with the corresponding ligaments poorly repairable. I plan to present a different viewpoint below. The common veterinary procedures of injecting with nonsteroidal anti-inflammatory agents, corticosteroids, hyaluronic acid and polysulfated glycosaminoglycans (Adequan) has been standard operating procedure for many years now. I view this as simply palliative care, doing little to cure the disease and quite possibly doing more harm than good! I particularly detest corticosteriods.
This page is principally interested in equine secondary Degenerative Joint Disease (DJD) involving progressive damage to the articular cartilage / joint from a primary insult. The question will be, what is this primary insult that starts the ball rolling and is there more going on under the hide than we generally suspect? What do vets think cause arthritic joints in the racehorse? DJD causes are generally believed to be precipitated from injury, genetics, over-work. and occasionally infections.
As with most things in medicine, it may be best to switch our study to human medicine for a bit to gain a deeper understanding on what arthritis may be in the horse. Human arthritis has been extensively studied and is considered one of our oldest diseases in our recorded history. Signs of it can be seen in bone dating back to prehistoric times. Arthritis has always been prevalent in our human populations, ever growing, afflicting the young as well as the old. There are hundreds of forms of human arthritis that affect a large segment of the population and this number grows every year. Lets stand back and take a deep breath questioning what the establishment tells us about arthritis and try to observe what may be actually happening?
The first clue to what may be going on is that arthritis has been ever with us for thousands of years showing no signs of disappearing. The same is true for the horse. The CDC states that 1 in every 250 children and 1 in every 5 adults in the USA will be diagnosed with arthritis. Two thirds of the people with arthritis are under age 65. The USDA conducted a study showing that 50% of lameness in a population of horses could be traced directly to joint pathology. As I have written in another part of this site, Dr. Paul Ewald and Dr. Gregory Cochran may be able to offer some insight into this. Dr. Cochran has been quoted as saying that widespread, old diseases are infectious, if their incidence in the general population is above one-in-one thousand. Likewise, if he sees a disease that has been observed in a population for many years, he becomes very suspicious that it may well be infectious in nature. His view is that the most "fitness antagonistic diseases" must be of an infectious nature as opposed to genetic. The word, "Fitness", is defined as simply the survivability of an animal over others on an evolutionary scale. Judith Hooper writes: "Consider a disease with a fitness cost of one percent -- that is, a disease that takes a toll on survival or reproduction such that people who have it, end up with one percent fewer offspring, on average, than the general population. That small amount adds up. If you have an inherited disease with a one percent fitness cost, in the next generation there will be 99 percent of the original number in the gene pool. Eventually the number of people with the disease will dwindle to close to zero -- or, more precisely, to the rate produced by random genetic mutations: about one in 50,000 to one in 100,000."
Dr. Ewald has come to the same conclusion that when one finds diseases in populations for many generations which still have a negative impact on fitness--they likely are infection based. Heritability has been discussed a lot with regard to arthritis. Note that the idea that certain diseases are heritable, common to family ancestors as arthritis is often described, may be an illusion. One can have transference of infections or pathogenic DNA/RNA from one generation to the other, giving all the appearance of being a natural heritable process as far as such processes can be described as "natural". The true genetic diseases tend to disappear in the future generations opposed to the generation-after-generation infections which linger. Ewald writes: "A disease-causing gene that reduces survival and reproduction would normally eliminate itself over a number of generations." Natural selection will weed out any defects that are not advantageous to that individual and the family lineage. This is not particularly true of an inherited infection. An infection will be manifested, generation-after-generation, damn the fitness costs and natural selection.
Furthermore, it appears little appreciated by both the geneticists and the medical men who value genetic mapping that our and our horse's DNA is not what it seems. It is not totally ours! Just because there are specific genes on our DNA code does not mean we were born with them nor that they are human or equine in origin! Microbes have long learned how to insert their genes into ours resulting in much "junk" DNA on our chromosomes. Viruses are well known for doing this, bacteria and fungi, not so much, but they can be quite adept. Amy Proal in her article, The Bacteria Boom, writes: "So there is increasing evidence that many of the genetic mutations identified by Human Genome Project researchers are largely induced by bacteria and other pathogens. Rather than serving as markers of particular diseases, such mutations generally mark the presence of those pathogens capable of affecting DNA transcription and translation in the nucleus. This is why, in most cases, the "one gene, one disease" hypothesis has failed to hold water. Instead, geneticists are now stuck examining a perplexing number of different mutations, most of which differ so greatly between individuals that no correlation can be made between their presence and any particular illness. The mutations are nothing but genetic "noise," induced either by random chance or by the pathogens that such researchers fail to factor into the picture."
I could not state this conundrum more elegantly! In short, she is saying that what our medical researchers like to suggest are purely genetic markers for a disease from random mutations could quite likely be caused by an infection from a microorganism that can manipulate our genes or insert their own genes into ours or our animal's chromosome-a mind boggling premise!

So if all of this is true, arthritis most likely has more of a microbial component which is often not appreciated!
I next will look at the life work of Thomas McPherson Brown MD for giving further insight into the legitimacy of this concept. The pathogenic theory behind inflammatory arthritis has been around a long time. The problem why this theory goes in and out of popularity can be traced to the Koch Postulates which is the golden test used by medicine to link an infectious pathogen to a disease:
(1) it must be found in all cases of the disease;
(2) it must be isolated from the host and grown in pure culture;
(3) it must reproduce the original disease when introduced into a susceptible host;
(4) it must be found present in the experimental host so infected
Though various microbes have been linked to inflammatory arthritis, many are discounted because the Koch postulates cannot be fulfilled. Big mistake! Microbiologists that specialize in L-forms (lacking a cell wall) of microbial life know that many times the Koch postulates will not apply. Same holds true for the mycoplasma class. Also, many times, these joint pathogens seem to be pleomorphic which means, they change shape which can really confuse many researchers, and mycoplasma is nearly invisible once it enters a cell. Put this all together and you have some of the reasons why infections are hard to identify in joints and why the infectious theory of arthritis is still very controversial!
Going back to the Koch Postulates with L-forms and Mycoplasma infections in mind what do we find:
1) If the practitioner is observant, the L forms which look like fried eggs can be seen many times in infected tissue but can easily be over-looked. Mycoplasma is virtually invisible to the microscope.
2) Both L-forms and Mycoplasma can be isolated, but growing them in culture media can be very tricky and is fraught with many mishaps when performed by the very best lab techs. Then are not easily grown and delicate!
3) The L-forms and mycoplasma will reproduce the disease only when the proper stimuli is present in the host. The immune system often must be weak, stress and injury may also be factors for the disease to manifest.
4) Finding it in the introduced host that developed the disease can also be elusive. Spirochetes for instance are very hard to isolate even in the acute phase which has a narrow window. Same holds true for L-forms and mycoplasma detection.
Dr. Brown begin his research in the 1930s working at the Rockefeller Institute examining joint fluid for infectious organisms that were smaller than common bacteria, since the larger bacteria had never been routinely found in what was considered a sterile joint capsule. Brown felt something must exist that every one was missing. His work eventually pointed to a possible mycoplasma infection which he managed to isolate from human joint fluid after much difficulty and toil. During this time, his lab floor neighbor, the famous Dr. Albert Sabin mentioned to Brown that he had isolated mycoplasma in the brain of a mouse infected with toxoplasmosis. He said he nearly missed this mycoplasma infection with normal microscope staining procedures. Sabin injected the mycoplasma infected mouse fluid into a second mouse who developed arthritis! Sabin felt this would be of interest to Brown's work. Mycoplasma seemed easy to identify and isolate in the genital tract of many animals, but when looking in other places, not so much. This is similar to the horse. Mycoplasma infection is the equine genital tract is widely written about in the veterinary literature, not in other places and certainly not equine joints!
Dr. Brown generally believed that basically three pathogen types were widely involved in inducing inflammatory arthritis. These are (1) spirochetes (as in Lyme disease), (2) streptococcus bacteria & L-forms, and (3) mycoplasma. All have a strong affinity to localize in joint capsules. Also, you have the perviously mentioned L-forms that lack cell walls but are derived from bacteria such as streptococcus which normally possess cell walls. This being opposed to the mycoplasma that are also cell wall-less, but they are not derived from a cell walled parent version like the L-forms. Many forms of bacteria and this is particularly true of streptococcus, can revert to a cell wall-less form (L-form) if the bacterium is stressed with antibiotics and other stimuli. This can be the normal cell-walled bacteria's response to saving itself from a pending danger such as coming in contact with an antibiotic and when that danger passes with the removal of the antibiotic or the immune system weakens perhaps by a use of corticosteroids, the L-form may easily revert back to the cell walled version that can cause another episode of the disease.
Dr. Brown developed an effective arthritis protocol that involved giving the antibiotic tetracycline orally or intravenously for mycoplasma infections. Oxytetracycline, erthromycin, vibramycin, clindmycin may also be used in patients that tolerate these better. Ampicillin is used if a streptococcus presence is suspected rather than mycoplasma. The tetracycline family of antibiotics are different from others like penicillin or ampicillin in that it does not act on the cell wall but on the inner physiology of the organism. This is why ampiciliin is used for normal streptococcus infections because they do normally possess cell walls. Not so mycoplasma.
Dr. Lida Mattman in her work, Cell Wall Deficient Forms wrote a whole chapter on joint infections and their vulnerability to L-forms of bacteria and mycoplasma. She writes: "Evidence of CWD forms (L-forms) play a significant role in infections of joint and osseous tissue is steadily accumulating. Incriminated variants include gonococci, staphylococci, clostridia, salmonella, corynebactreria, and perhaps most importantly, propionibacteria. " She found it was very important to have the proper culture media if one wanted to successfully isolate and grow L-forms and Mycoplasma. In the veterinary joint section, she writes that 23 samples of sterile joint fluid cultured in the veterinary lab produced growth when L-form and mycoplasma media were used with L-forms being implicated in domestic animal joints on a constant basis.

Next, I would like to examine the work of Dr. Robert Becker, MD. He is known for his groundbreaking research into bone remodeling which will play an important role in the protocol I suggest for healing arthritic joints in the racehorse. In his book, The Body Electric, he described his discovery when a positively charged silver electrode was introduced into damaged tissue resulting in embryonic stem cell formation.
Dr. Becker believes that there are three stages to this silver ion protocol:
1) Silver ions driven by a positive low voltage current deactivates bacteria, fungi in the infected area,
2) Silver ions acts on the fibroblast cells reverting them into embryonic like stem cells,
3) Formation in vivo of an adequate blastema to support regeneration of previously damaged tissue.
From his explanation of the mechanism: "Electrically-generated silver ions from the anode penetrate into the adjacent tissues and undergo a series of three reactions. First, the silver ions combine with proteins, peptides and various other chemical species normally present in solution in the tissues. The silver ions also combine with any bacteria, fungi or viruses present in the treatment area. If treatment is continued after all or most available sites for this type of reaction have been exhausted, the newly-generated silver ions associate with cells in the region, particularly fibroblast cells and epithelial cells, resulting in de-differentiation of these cells into embryonic cell types. Then, if treatment is continued after this second reaction is substantially complete, the free silver ions form a complex with collagen fibers present in the wound. This silver-collagen complex is believed to act as a biological inducer to activate the previously-produced de-differentiated fibroblast or epidermal cells to multiply and produce an adequate blastema."
With a blastema present, regeneration of the damage structure is possible!
Dr Becker writes in his patent on the procedure which he is trying to stimulate regeneration:
The most effective--and most complex--type of healing is regeneration. This type of healing is capable of replacing entire limbs and internal organs, and even portions of the brain and heart. Regeneration is a biphasic process. In the first phase, normal, mature cells at the site of the injury revert to an embryonic, unspecialized form ("de-differentiate"). These cells multiply rapidly, then become activated and demonstrate a variety of energetic processes which may include amitotic division, nuclear transfer, migration of free nuclei into residual tissues, and production of exceptionally large cells containing nuclear material from a number of individual de-differentiated cells (thus, "activated cells" are cells that undergo these processes). Activation results in the rapid accumulation of a large mass of embryonic cells known as the blastema, which is the essential element for regeneration. The blastema may be viewed as providing the biological raw material needed for rebuilding the missing tissues: formation of an adequate blastema results in complete regeneration of the missing tissues, whereas if the blastema is inadequate in size, only partial or incomplete regeneration takes place (formation of a stunted or incomplete part, or merely regeneration of individual tissue types that are not fully organized into the desired structure).
In the second phase of the regeneration process, the embryonic cells of the blastema respecialize ("re-differentiate") into the various types of cells needed to rebuild the missing tissues and organized structures in complete anatomical detail. The rebuilding process is essentially a recapitulation (albeit on a local scale) of the original embryonic development of the tissues being replaced.
To summarize this section on Dr. Becker's work, I would like to first say regeneration does happen in the higher mammals, if on a limited scale. It is a little known fact that children under the age of 12 often have the power to naturally regenerate finger tips that have been completely severed in an accident, if properly managed. This phenomena has been observed hundreds of times and it is a true regeneration with a blastema appearing resulting in bone, cartilage, tendon, blood vessels, skin, nail, cuticle, fingerprint, and nerve formation. The key why young mammals have this regenerative power and others don't may lay with electrical stimulation or a neuroepidermal junction stimulation stimulating the formation of many despecialized blastemal cells in the region.
Becker writes: "It (silver) stimulates bone forming cells, cures the most stubborn infections of all kinds of bacteria, and stimulates healing in skin and other soft tissues. Most important of all, the technique makes it possible to produce large numbers of dedifferentiated cells, overcoming the main problem of mammalian regeneration---the limited number of bone marrow cells that dedifferentiate in response to electrical current alone. Whatever its precise mode of action may be, the electrically generated silver ion can produce enough cells for human blastemas; it has restored my belief that full regeneration of limbs and perhaps other body parts can be accomplished in humans."
A work in progress, tune back for the completion.
My suggested Regenerative Joint Protocol:

Low Level Laser therapy (LLLT) has some unique benefits when it comes to treating damaged joints. It is not a very well know fact that laser can not only activate stem cells in the body, but attract them to the area where the laser radiates. Recent work done at Harvard demonstrated that LLLT can stimulate the stem cells in a rat's damaged molar into new tooth regeneration. They found that LLLT treatment generated a reactive oxygen species (ROS). ROS stimulated dentin production by activating transforming growth factor beta (TGF-β) which stimulates a signaling protein resulting in stem cell differentiation.
Effect of low‐level laser therapy on bone repair: Histological study in rats
Abstract
Bone remodeling is characterized as a cyclic and lengthy process. It is currently accepted that not only this dynamics is triggered by a biological process, but also biochemical, electrical, and mechanical stimuli are key factors for the maintenance of bone tissue. The hypothesis that low-level laser therapy (LLLT) may favor bone repair has been suggested. The purpose of this study was to evaluate the bone repair in defects created in rat lower jaws after stimulation with infrared LLLT directly on the injured tissue. Bone defects were prepared on the mandibles of 30 Holtzman rats allocated in two groups (n = 15), which were divided in three evaluation period (15, 45, and 60 days), with five animals each. control group-no treatment of the defect; laser group-single laser irradiation with a GaAlAs semiconductor diode laser device (lambda = 780 nm; P = 35 mW; t = 40 s; Theta = 1.0 mm; D = 178 J/cm(2); E = 1.4 J) directly on the defect area. The rats were sacrificed at the pre-established periods and the mandibles were removed and processed for staining with hematoxylin and eosin, Masson's Trichrome and picrosirius techniques. The histological results showed bone formation in both groups. However, the laser group exhibited an advanced tissue response compared to the control group, abbreviating the initial inflammatory reaction and promoting rapid new bone matrix formation at 15 and 45 days (P<0.05). On the other hand, there were no significant differences between the groups at 60 days. The use of infrared LLLT directly to the injured tissue showed a biostimulating effect on bone remodeling by stimulating the modulation of the initial inflammatory response and anticipating the resolution to normal conditions at the earlier periods. However, there were no differences between the groups at 60 days.
Low-level laser therapy: a useful technique for enhancing the proliferation of various cultured cells
Khalid M. AlGhamdi & Ashok Kumar & Noura A. Moussa
Abstract
The aim of this work is to review the available literature on the details of low-level laser therapy (LLLT) use for the enhancement of the proliferation of various cultured cell lines including stem cells. A cell culture is one of the most useful techniques in science, particularly in the production of viral vaccines and hybrid cell lines. However, the growth rate of some of the much-needed mammalian cells is slow. LLLT can enhance the proliferation rate of various cell lines. Literature review from 1923 to 2010. By investigating the outcome of LLLT on cell cultures, many articles report that it produces higher rates of ATP, RNA, and DNA synthesis in stem cells and other cell lines. Thus, LLLT improves the proliferation of the cells without causing any cytotoxic effects. Mainly, helium neon and gallium-aluminum-arsenide (Ga-Al-As) lasers are used for LLLT on cultured cells. The results of LLLT also vary according to the applied energy density and wavelengths to which the target cells are subjected. This review suggests that an energy density value of 0.5 to 4.0 J/cm2 and avisible spectrum ranging from 600 to 700 nm of LLLT are very helpful in enhancing the proliferation rate of various cell lines. With the appropriate use of LLLT, the proliferation rate of cultured cells, including stem cells, can be increased, which would be very useful in tissue engineering and regenerative medicine.